From the very early days of the COVID-19 outbreak, public, private and university researchers have been working to develop vaccines. There are now ten such vaccines being administered worldwide, with Russian and Chinese governments producing public sector-led versions, Oxford University developing AstraZeneca, and the private sector coming forward with the Moderna, Pfizer, and J&J products, these latter the most widely tested, certified and applied in the Western world. Optimism that we may yet overcome this pandemic is on the rise, but could it be misplaced?
Some of the vaccines are produced using a first time ever, new mRNA technique, others are produced the old-fashioned way, but whichever way, the results, and speed from research, development, to production, has been nothing short of a miracle. While not a “silver bullet”, virtually all knowledgeable experts see wide-scale vaccination as the major weapon in stunting if not reversing pandemic expansion. It is fair to say we are at the dawn of the “New Vaccine Era”.
This plethora of vaccine options has created optimism, suspicion, and anger over inequity for countries and individuals.
Optimism on the Rise: End of the Pandemic in Sight?
Because many countries are achieving or planning to achieve high levels of vaccinated populations in order to reach some form of “herd immunity”, optimism is spreading.
Since February 2021, Israel has the highest vaccination rate followed by the United Arab Emirates; as of 6 April, aside from Israel that still leads the pack, the country rankings have changed, as shown by this chart prepared by the University of Oxford’s Our World in Data project:
The daily “push” to get as many people vaccinated as possible varies by country, but the latest data (6 April) shows Israel still ahead of everyone, followed by the United Arab Emirates, Chile, the United Kingdom, and the United States:
That is just the tip of the iceberg: There are huge gaps between vaccination programs in different countries and divides between continents.
Some countries and regions which should be doing better, aren’t. Notably, Western Europe has been experiencing unjustified delays that have resulted in a “Vaccine Mess” – all the more unjustified that some European countries, particularly France, Italy and Germany, have public health systems with a stellar reputation. A reputation that European citizens, however, are now coming to realize is no longer justified: In fact, neoliberal austerity policies and misguided attempts to “contain” public debt over the last decade have damaged their effectiveness. For example, in response to demands to cut public funding, Italy has systematically shut down small hospitals that served rural areas and as a result, when COVID-19 hit, the country found itself short of beds for pandemic victims.
Then there is the United States. After a very bad beginning with the numbers of cases and deaths remaining the highest in the world, the United States has been rapidly expanding vaccinations with prospects of more than 200 million by the end of April 2021.

Optimism from the individual’s perspective, both in countries with robust vaccination programs and those without, is because there is a sense that “help is on the way”. This is what was desperately needed for most of 2020, and now seems to be taking hold.
But Suspicion Is Also Spreading
Because of the speed with which these vaccines have come onstream, mistrust exploded, a result of past bad experiences with government vaccine approvals, and insufficient time allowed to conduct trials on various cohorts. Indeed, the Government of Netherlands suspended use of AstraZeneca at least in part because of instances of blood clotting in different populations, including pregnant women.
The AstraZeneca saga is far from over. On 8 April, EMA underlined that a link between the vaccine and very rare forms of thrombosis did indeed exist, but it reiterated that the benefits outweighed the risks, leaving the choice of any limitations to individual countries. Italy, for example, immediately took the decision to limit the vaccine to over-60s. The UK has already gone ahead with suspension for under-30s and so have the Netherlands and Germany.
Further, and more worryingly, AstraZeneca made a significant blunder in early-on releasing efficacy data that was too high which undermined trust in its reliability, and indirectly in vaccines writ large. And most recently, J&J had to discard 15 million vaccines because of a production error in Baltimore, Maryland.
Suspicion has also been exacerbated because public officials have sent confusing messages about what is mandated, what they can do voluntarily, and/or what the science dictates.
The United States shows how bad it can get: An ex-President and many of his most vocal advisors made and continue to cast doubt about the need for a vaccine, complemented with mockery of wearing face masks. President Biden has been assiduously expressing reliance on what the “science” tells him; he got vaccinated and always wears a mask. Yet, some sub-national leaders talk and do the very contrary with anti-science rhetoric.
But even when a President turns away from the politically and economically expedient to rely on the scientific, there is still confusion.
The U.S. Centers for Disease Control and Prevention (US CDC) is the national authoritative voice on this, but its messaging has been changing almost on a daily basis with respect to safe levels of social interaction when vaccinated, when schools can safely open, where and when does it remain necessary to wear a mask. The U.S. CDC website guidance has become a sort of “breaking news”, making it harder for institutions and individuals to know what to do.
The European Union is no better and disunited despite the European Centers for Disease Control and Prevention (ECDC). In theory “All countries in the EU have responded to the situation by implementing a comprehensive package of measures, including surveillance, testing, increased hospital and isolation capacity, contact tracing, case management and strategies to mitigate the impact of the pandemic, such as physical distancing measures.”
But without addressing Member State compliance or noncompliance, the ECDC website notes:
“Transmission is still widespread in the EU/EEA. It is possible that further increases in admissions to hospital, ICU and mortality will follow in the coming weeks in those countries that are currently observing increasing case notification rates. Hence, it is still important to maintain public health and physical distancing measures.”
Furthermore, Europe is awash with national medical centers designed to monitor diseases and guide vaccination policies, plus, of course, a European-level institution, the European Medicines Agency (EMA) tasked, inter alia, with approving COVID vaccines. Over the AstraZeneca COVID vaccine, the confusion reached absurd levels, with the German medicines center advising suspension of the vaccine (due to a suspicious series of thrombosis cases) with, as a result, a majority of European countries following suit, while EMA continued to advocate vaccination, arguing that the benefits were too large to pass up.
It would appear that there is an urgent need for Europe to pull its act together and decide once and for all who does what: the EMA, the ECDC or the national medical centers. We all know that COVID-19 is likely the first pandemic of this century and that many more are in the offing. A confused institutional structure for public health is the last thing any country or group of countries (like the EU) should have.
And Anger over Inequities Explodes
Vaccination has further divided the world, and the distance between the haves and have-nots has never been greater as billions of people are left without any prospect of getting vaccinated anytime soon. Predictably this has led to an outcry over the inequity all this has caused.
However, it is not just a matter of equity or lack thereof. There is serious medical evidence that allowing free rein for the COVID virus to spread in an uncontrolled manner in the developing world means increasing the chances of one or more variants emerging. At the time of writing, the situation in Brazil and India is fast becoming dramatic:
This in turn threatens the efficacy of currently available vaccines, even if (so far) pharmaceutical companies have had nothing but reassuring words about the efficacy of their vaccines.
But the threat is there and cannot be denied. And the conclusion is clear: Unless the whole world is vaccinated in such a way that herd immunity kicks in, we remain at the mercy of possible virus variants that present vaccines cannot control.
Vaccine manufacturers will need to address COVID variants and both national and regional public health institutions need to issue guidance in this respect. In short, it has become an urgent public health priority to define an expedited regulatory process for the adaptation of vaccines to protect against current or future variants. The European Union has just started to invest in COVID variants research:
📢 Great news in our fight against #coronavirus!
Today we are mobilising €123 million from #HorizonEU to further support urgently needed #research & #innovation to tackle #COVID19 & its variants! 🩺
➡️ https://t.co/tA99Y2osfu@EU_Health #ResearchInfrastructures #worldhealthday pic.twitter.com/IRaUVFWDAp
— Mariya Gabriel (@GabrielMariya) April 7, 2021
There are ongoing discussions at the regional level in Europe – and this involves EMA – on how to approach variants and vaccines in a coordinated way. But this is also something that should be done on an international level with the engagement of all willing national Centers for Disease Control and Prevention.
The neoliberal ideology that calls for a full-throated defense of intellectual property and patents (the idea is to defend innovation) has so far guided the reaction of many large vaccine manufacturers. As a result, much of the private sector pharmaceutical industry, supported by those countries with strong pharmaceutical private sectors, has not been prepared to require companies to make their vaccine formulas available to other producers.
To date, it has translated into limiting access principally to those who can pay for it, or have sufficient political leverage to gain access. What happens, in essence, is that many developing countries are denied coverage.
A Washington Post article spells out the consequences of such an approach, pointing out that “Billions of people are left with an uncertain wait, with most of Africa and parts of South America and Asia not expected to achieve widespread vaccination coverage until 2023, according to some estimates.” And the vaccine manufacturers maintain that “the rapid development of new vaccines” are in fact “evidence that the drug industry’s traditional business model, based on exclusive patents and know-how, is working.”
Claims that the system is working are not credible in the face of billions of unvaccinated people who won’t (or can’t) be protected before 2023 if business goes on as usual.
But things, they are a-changin’: hope is coming from the international community. The creation of COVAX, an international multi-partner financing mechanism to provide the money and the wherewithal to both obtain and administer vaccines in developing countries, is garnering new traction. The European Union has always been in the forefront supporting COVAX:
#COVAX has now delivered vaccines to 100 countries.
This is a real milestone. I’m proud of #TeamEurope‘s contribution to this global effort of solidarity.
Our common fight against #COVID19 continues, to make sure no one is left behind. pic.twitter.com/Xz9qqkC3aw
— Ursula von der Leyen (@vonderleyen) April 8, 2021
And now that Trump has left the scene, both President Biden and Prime Minister Johnson have announced substantial, in fact, game-changing increases in contributions. COVAX. The Center for Global Development’s executive vice president Amanda Glassman, a global health expert and former principal technical lead for health at the Inter-American Development Bank, welcomed them with the following statement:
“The Biden Administration’s move to commit $4 billion to COVAX is a long-overdue step toward ending the pandemic globally, especially since the rise of new variants means that the only way to truly control COVID is to make sure everyone can get vaccinated—not just people in rich countries.”
The major international financial institutions are now well aware of the damages of this pandemic, and that it will not be contained until many people, worldwide, are vaccinated. At the World Bank Group and IMF Spring Meetings which will end this week, it has been on the leaders’ minds, taking into consideration ideas proffered by both insiders and outsiders as to how to significantly ramp up COVAX’s funding and reach, and well beyond.
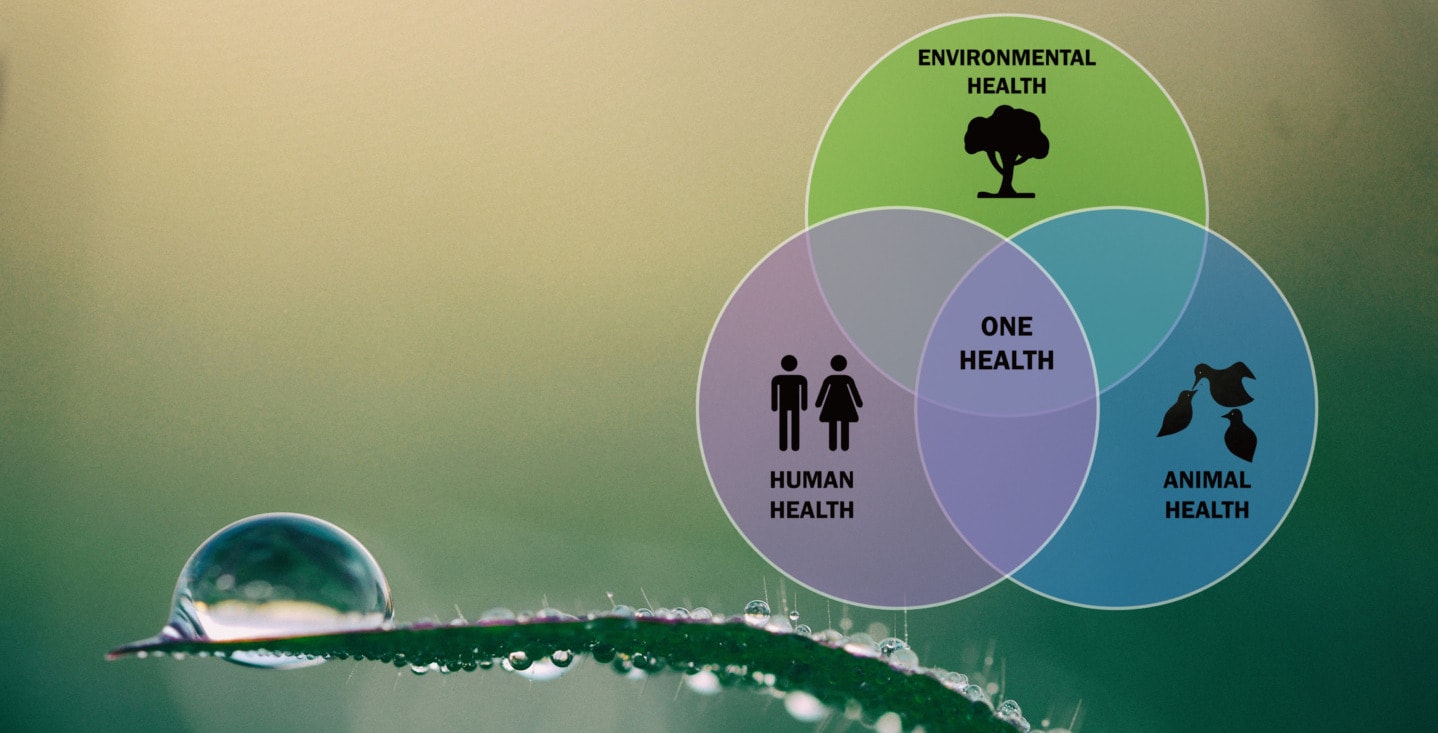
The Rockefeller Foundation, in particular, issued a 22-page report whose contributors included former UK Prime Minister Gordon Brown and Columbia U. Professor Jeffrey Sachs, urging the IMF to approve and swiftly distribute $650 billion in additional reserve assets to help developing countries vaccinate as much as 70% of their population by the end of next year. “Any plan should incorporate strategies to mitigate the risk of future pandemics by addressing ongoing microbial threats, including antimicrobial resistance,” said Olga Jonas, a senior fellow at the Harvard Global Health Institute. “What is really needed is an urgent plan for robust core veterinary and human public-health systems in all low- and middle-income countries.”
The Vaccines’ Next Chapter: Is There Hope?
The vaccine research story is an ongoing one, with prospects of new delivery systems being researched and developed by the public, private, and not-for-profit sectors. For example, CEPI, another part of the international multi-partnership, is providing financing to a University of Hong Kong effort to bring an intranasal vaccine into the mix.
An Israeli company has indicated an oral COVID-19 vaccine should become available in a reasonably short time. The advantage is obvious: people could self-vaccinate at home.
Moderna has announced that it is creating a combination flu-COVID vaccine. With the same mRNA technology, it plans to target the seasonal flu, Nipah virus, and HIV. That would definitely be an extraordinary time-saver, accelerating vaccine distribution the world over.
Perhaps the most exciting discovery is the brainchild of Jason McLellan, a structural biologist at the University of Texas at Austin, considered by many a genius. This is not his first discovery but the latest in a string of discoveries that are the basis of the new much-touted mRNA technology. He identified a six-spike protein that he dubbed Hexapro: Once inserted into a vaccine, it could make it far more potent than current COVID vaccines and far cheaper to produce.
The new vaccine, called NDV-HXP-S, is now entering clinical trials in Brazil, Mexico, Thailand, and Vietnam. If it proves safe and effective (for now it has shown to work for mice), then it could be produced very cheaply in the billions of doses. This is so, because contrary to current vaccines, NVD-HXP-S can be mass-produced in chicken eggs using widespread, available know-how in existing flu vaccine factories in countries like Vietnam, Brazil, or India. As Andrea Taylor, assistant director of the Duke Global Health Innovation Center says: “That’s staggering — it would be a game-changer.”
And there are many other researchers still at it, ones which have not yet gone public but are ongoing. It is fair to conclude that, if the past is a prologue to our future, and therefore how we deal with COVID-19 will determine how well we will address future pandemics, then perhaps, all hope is not lost. Consider that if innovations keep pouring in, we won’t need to fear the future as much as we did in 2020 or even today. Still, a very big if.
Editor’s Note: The opinions expressed here by Impakter.com columnists are their own, not those of Impakter.com — Featured Image Credit: Alex Mecl on Unsplash