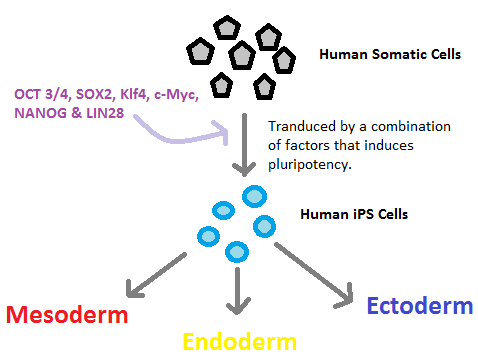
The scientific benefits of stem cell research are often overshadowed by pro-life arguments against using embryonic matter in such exploration. However, what many individuals do not realize is that the ability to induce pluripotent stem cells or iPSCs (according to Merriam Webster, these are cells – either immature or stem cells – that can give rise to several different cell types) has provided scientists with what seems to be a viable alternative to using embryonic matter in their research by eliminating the ethical concerns associated therewith.
Critics of stem cell research often take the form of hyper-conservative individuals relying upon faith-based reasoning – these people tend to voice a blanket opposition toward all stem cell research, mainly due to a misconception that such research necessarily uses embryonic stem cells. However, in 2006, Kazutoshi Takahashi and Shinya Yamanaka created a game-changing alternative with similar research potential – the induced pluripotent stem cell, which can give rise to most, if not all, 200 types of cells in the body. Prior to Drs. Takahashi and Yamanaka’s work, pluripotent stem cells were only obtained from the embryo’s inner stem cell mass.
In the Photo: the ability to induce pluripotent stem cells or iPSCs has provided scientists with what seems to be a viable alternative to using embryonic matter. Credit: By Humanips (Own work) via Wikimedia Commons [CC BY-SA 3.0]
Today, many research institutes and biotechnology companies have adopted the use of induced pluripotent stem cells (iPSCs) instead of using embryonic stem cells in research. According to the National Institutes of Health (NIH) within the United States’ Department of Health and Human Services, iPSCs are defined as “adult cells that have been genetically reprogrammed to an embryonic stem cell–like state by being forced to express genes and factors important for maintaining the defining properties of embryonic stem cells” – however, while the iPSCs behave like embryonic stem cells, they are in fact derived from adult cells.
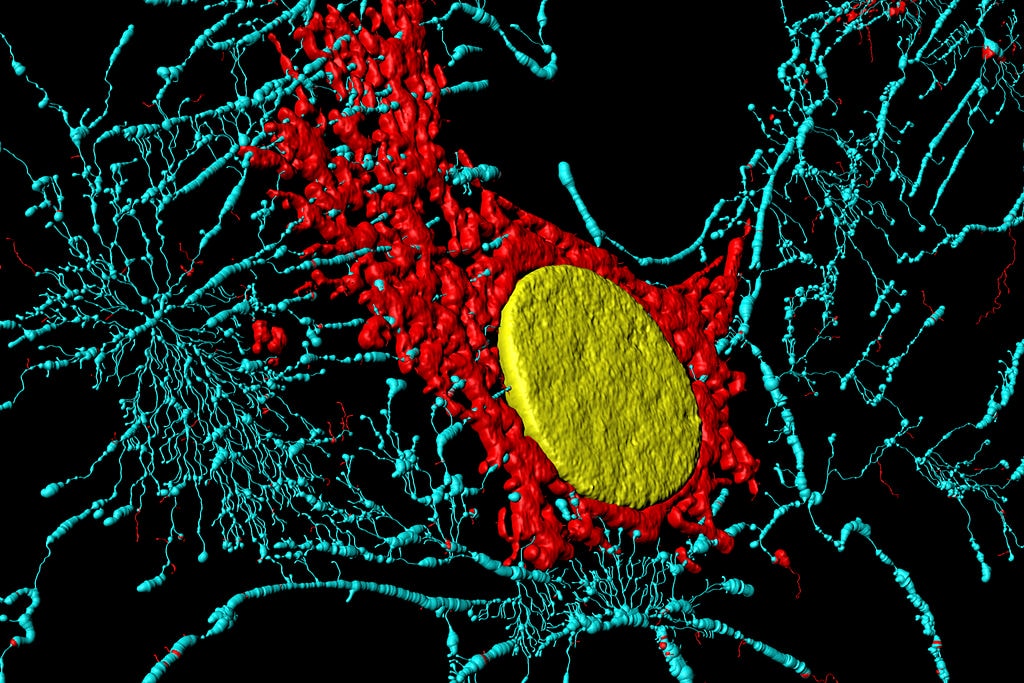
In their experiment, “[Takahashi and Yamanaka] reprogrammed mice fibroblast cells, which can produce only other fibroblast cells, to become pluripotent stem cells, which have the capacity to produce many different types of cells…They called the pluripotent stem cells that they produced induced pluripotent stem cells (iPSCs) because they had induced the adult cells, called differentiated cells, to become pluripotent stem cells through genetic manipulation.” iPSC technology has advanced the study of disease modeling at its core, and has created potential for cell-replacement therapy (especially in the cardiac and neuronal fields, though advances using iPSCs have been less rapid in the renal field).
In the Photo: Microfilaments, mitochondria and nucleus in fibroblast cells. Credit: Heiti Paves (Own work) [CC BY-SA 3.0], via Wikimedia Commons
In fact, the benefits to using iPSCs in research are ever-increasing –a December 2013 paper published in Cellular & Molecular Immunology found that among other potential utilizations, “[w]ith respect to potential applications in the immune system, many studies provide evidence to support that there are exclusive advantages to using iPSCs over other systems.” The necessity of continuing such exploration is undeniable. The potential implications for determining the genetic makeup of disease could transform immunotherapy, leading to previously uncontemplated advances in medicine. For example, iPSCs could help differentiate between individual patients given the same diagnosis, so as to better comprehend variations in individual patient responses with the same disease.
Related article: “IS BREASTFEEDING ALWAYS BEST?“
iPSCs have convinced a number of pro-life proponents of their use as acceptable in research and laboratories; however, the general public typically is unaware of the nuances and distinctions between embryonic stem cells and iPSCs and as such may have uninformed objections to their use. It is only through extensive education and clear-headed discussion in mainstream media that iPSCs and embryonic stem cells will no longer be synonymous in their usage when people think generally about stem cell research.
While it has not been established beyond a doubt that iPSCs can replace embryonic stem cells in research, there is significant evidence demonstrating that iPSCs do indeed strongly resemble embryonic stem cells, including “the[ir] ability to to differentiate from a blank slate to any of the 220 types of cells in the human body, and ability to reproduce indefinitely in culture.” In this sense, iPSCs are easier to create than embryonic stem cells; researchers can develop them in-house in any standard biology lab with obtainable materials (not human eggs or embryos).
In the Video: Scratch closure of fetal keratinocytes and fibroblasts in co-culture. Credit: By Zuliani T, Saiagh S, Knol A, Esbelin J, Dreno B [CC BY 2.5], via Wikimedia Commons.
Furthermore, the potential benefits from using iPSCs in research are enormous – first and foremost, the implications for disease treatment are enormous in that these cells can be reprogrammed into limitless immune compatible embryonic stem cells, for example, which could then be used to create various cells to treat innumerable diseases. A press release from UCLA shortly after Takahashi and Yamanaka’s discovery lists a few examples – beta islet cells to treat diabetes, hematopoietic cells to create a new blood supply for a leukemia patient or motor neuron cells to treat Parkinson’s disease.
For a full mindmap behind this article with articles, videos, and documents see #stemcells
From a bioethical standpoint, iPSCs do not fall prey to many of the same pro-life arguments utilized against using embryonic stem cells in research. One key difference between iPSCs and embryonic stem cells is, of course, the source of origin for each (from adult versus an embryo or human egg, respectively). Additionally, an iPSC cannot develop into a complete embryo (it lacks the the ability to generate the cell layers necessary to do so). While some argue that iPSCs could result in somatic cell nuclear transfer (cloning), this argument does not specifically apply to iPSCS; any adult stem cell could have a potential use for cloning.
Catholic pro-life bioethicist and blogger Rebecca Taylor, of Mary Meets Dolly, proffers the following differentiation between iPSCs and embryonic stem cells. She explains that in an experiment where scientists were able to grow a mouse solely using iPSCs, upon closer examination, the scientists also manipulated some of the iPSCs with a process called tetraploid complementation in order to create a human embryo capable. Because the iPSC could not have evolved into the embryo without intervention, she holds that this distinguishes iPSCs from embryonic stem cells and avoids the ethical issues associated with the latter.
Among the several objections that pro-life advocates have against the use of iPSCs in stem cell research, Taylor indicates that only one seems to hold water as a true concern for pro-life advocates – that iPSCs developed from embryonic fetal tissue: the use of HEK 293 in the reprogramming of adult cells back to pluripotency. Taylor explains that the viruses used in the reprogramming are grown from HEK 293, which in turn was derived from an aborted fetus’ kidney tissue back in the 1970s. On the other hand, others, including the Center for Bioethics and Cultural Network President Jennifer Lahl, argue that while leading to the development of iPSCs, many of the early experiments did in fact use fetal tissue to grow viruses used in iPSC creation, this was simply a convenience given the times. These experiments would have garnered the same results had adult DNA or tissue been used, and the fetal tissue was a non-essential part of iPSC creation, which makes the use of HEK 293 and viruses derived from it a weak argument against the use of iPSCs in stem cell research.
To summarize, iPSCs may provide the perfect solution for any ethical objections to stem cell research on the grounds that embryonic cells are utilized. Stem cell research is an essential component of regenerative medicine, with the potential for exponential growth in successful disease treatment. However, there remains a significant amount of research that must be done before scientists can successfully realize the full therapeutic potential of adult stem cells. In order to move forward with the necessary experimentation to take full advantage of the potential benefits of iPSCs, it is imperative that individuals with ethical objections to all stem cell treatment clearly understand the distinction between induced pluripotent stem cells and embryonic stem cells.
Upon closer analysis, nearly all of the pro-life objections to the use of iPSCs are invalidated and iPSCs appear to be the perfect solution for those with ethical objections to embryonic stem cell research.
Recommended reading: “SQUEEZING CELLS INTO STEM CELLS”
_ _