Healthcare is evolving faster than ever. New technologies, shifting patient needs, and emerging global health risks are transforming the way nurses and healthcare practitioners deliver care. In this changing environment, traditional training alone can’t keep up. Today’s professionals require forward-thinking educational approaches and a proactive mindset that prepare them not only to respond to current challenges but to anticipate those still on the horizon.
From evidence-based curricula to immersive simulation labs and telehealth training, modern education is reshaping how practitioners learn, think, and lead. For many clinicians seeking to confidently step into advanced roles, expanding their expertise through further education provides direct pathways to acquire the knowledge and clinical capabilities necessary to care for diverse populations and guide teams in unpredictable environments.
This article explores how smarter, innovative education is shaping a more prepared healthcare workforce that is capable of delivering high-quality care in a rapidly changing world.
The urgent need for modernized healthcare training
The demands on today’s healthcare professionals are dramatically different from what they were even a decade ago. Chronic diseases are rising, populations are aging, and new infectious threats can appear overnight. At the same time, healthcare organizations are adopting digital systems, remote-care models, and advanced medical technologies that require new competencies.
Clinicians are now expected to navigate telehealth platforms, analyze data for clinical decision-making, collaborate within increasingly complex interdisciplinary teams, respond to emerging public health crises, and lead care initiatives rooted in evidence and quality improvement principles.
This growing list of expectations means that education programs must evolve fast. Fortunately, many nursing schools, health sciences departments, and online degree providers have completely redesigned their training models to better reflect the realities of modern practice. These changes not only help practitioners meet current demands but also prepare them to adapt quickly as new technologies, public health patterns, and patient expectations emerge.
Building smarter curricula through evidence-based education
Forward-thinking nursing and healthcare programs are no longer relying on static course outlines. Instead, they use evidence-based curricula that reflect the latest research on patient care, safety standards, and clinical best practices.
This approach ensures that learners are taught updated protocols, real-world clinical decision frameworks, evidence-supported interventions, and skills for evaluating research and applying it to practice.
Evidence-based education supports a more agile workforce, empowering practitioners to adjust their approach as new information becomes available, which is critical in a field where guidelines can shift overnight due to emerging diseases or new scientific findings.
The future of clinical readiness

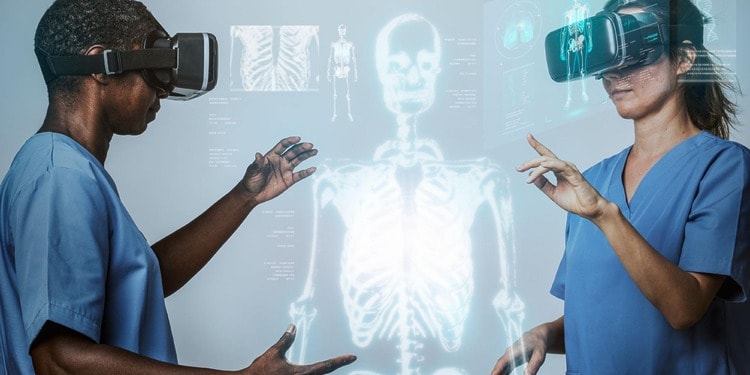
Simulation has become a cornerstone of advanced healthcare training, and for good reason. Modern simulation labs use high-fidelity mannequins, digital monitoring systems, augmented reality, and team-based practice scenarios to mimic real clinical environments.
These experiences offer benefits that traditional clinical rotations often cannot. Benefits include:
Safe and controlled learning
Students can rehearse complex procedures, respond to emergencies, and practice communication without risking patient safety.
Exposure to rare but high-risk scenarios
Events like cardiac arrest in a newborn or sudden anaphylaxis are unpredictable in real clinical practice but can be simulated with precision.
Team-based communication training
Simulation strengthens collaborative skills between nurses, physicians, and other professionals, improving coordination in real-world care.
Immediate feedback
Instructors can pause a scenario to provide coaching or conduct debriefs that help students reflect, correct errors, and build confidence.
As healthcare systems continue to face workforce shortages and increased patient acuity, simulation ensures new practitioners enter the field better prepared and more capable from day one. It also helps bridge the gap between academic learning and real clinical environments, giving students the chance to build confidence before interacting with patients in high-pressure settings.
Telehealth training for a digital future
Telehealth has become an essential component of healthcare delivery, particularly in rural and underserved communities. As digital care becomes more mainstream, clinicians must learn how to provide high-quality, patient-centered care through virtual platforms.
Modern healthcare programs now include telehealth content such as conducting remote physical assessments, establishing rapport and trust through a screen, using digital diagnostic tools, ensuring patient privacy and cybersecurity, managing chronic conditions remotely, and documenting digital care encounters accurately.
Developing these skills prepares practitioners to succeed in a healthcare landscape where virtual care is expected.
Preparing clinicians to guide change

The future of healthcare depends heavily on strong, adaptable leaders. That’s why progressive education programs weave leadership development not just in standalone courses, but throughout their curricula.
Nurses and practitioners are trained to lead interdisciplinary teams, navigate ethical dilemmas, coordinate care across multiple providers, advocate for evidence-based changes, communicate effectively with stakeholders, and drive quality improvement and patient safety initiatives.
Leadership skills are essential for advanced practice nurses, especially those who plan to guide community health efforts, operate clinics, or serve as primary care providers in areas where physician shortages are growing.
Why are many nurses turning to advanced online programs
As the need for highly skilled clinical leaders continues to rise, many nurses are choosing to advance their education through flexible online degree pathways.
Nurses looking to expand their expertise and meet future healthcare demands often choose an online FNP program, gaining the advanced knowledge and clinical skills needed to lead in their communities.
These programs offer:
- Flexible scheduling – ideal for working nurses balancing shifts, family, and career growth
- Access to experienced faculty – often practicing clinician-educators
- Simulation-integrated training – delivered through virtual or hybrid labs
- Telehealth competencies – built directly into the curriculum
- Leadership-focused coursework – preparing graduates for expanded roles
- Real-world clinical placements – arranged in students’ local communities
For many nurses, online learning provides the most accessible pathway to becoming a Family Nurse Practitioner, which is a role at the forefront of modern community-based healthcare delivery.
Smart education shapes a stronger healthcare future
Healthcare is changing, but with innovative education models, the workforce is rising to meet the challenge. Evidence-based teaching, cutting-edge simulation, telehealth training, and strong leadership development are creating practitioners who are adaptable, confident, and equipped to provide exceptional care no matter what tomorrow brings.
As advanced illness patterns, digital-care models, and community health needs continue to evolve, modern training will remain critical. Healthcare professionals who invest in forward-thinking education today will be the leaders shaping a more responsive, resilient, and patient-centered system in the years ahead.
Editor’s Note: The opinions expressed here by the authors are their own, not those of impakter.com — In the Cover: Health Challenges with Smarter Education and Training — Cover Photo Credit: Pixabay