Gun violence is a medical problem just like heart disease, but not for the reason you might expect.
On December 2nd of last year, news outlets across the United States reported an all-too-familiar headline: another mass shooting claimed American lives, this time in San Bernardino, California. The event reinvigorated the ever-smoldering American gun safety debate, with The Left calling for tighter restrictions, and The Right countering that such restrictions would only make matters worse.
Two weeks after the San Bernardino shooting, the American Heart Association released a report describing an alarming epidemic in the US. The report noted that a staggering 375,000 Americans died of heart disease last year, a figure that dwarfs the 33,636 gun deaths. And a closer look at the numbers reveals another important gap between heart disease and gun violence: while the data on heart disease is plentiful, the data on gun violence is full of holes. We just don’t research gun attacks like heart attacks.
But we should.
Congress stifled gun violence research in the US in the mid-1990s after pressure from the National Rifle Association (NRA). In 1993, a study funded by the Centers for Disease Control (CDC) showed a link between gun ownership and gun death. The subsequent NRA lobbying pressure ultimately led to a 1996 appropriations bill declaring that no CDC funds could be used to “advocate or promote gun control.” The bill reduced CDC funding for research on gun violence by 96% compared to levels in the mid-1990s, creating a data vacuum.
Related article: “OVER-TESTING WITH CT SCANS IN THE EMERGENCY DEPARTMENT”
Data on heart disease, in contrast, is readily available, allowing experts to refine their methods of tackling the problem. Researchers work to identify the best medications, diets, exercise regimens, awareness campaigns, and community engagement programs to better help people with heart disease. Then, with a wealth of research at their fingertips, a panel of experts called the Joint National Committee writes guidelines to ensure quality care across the US.
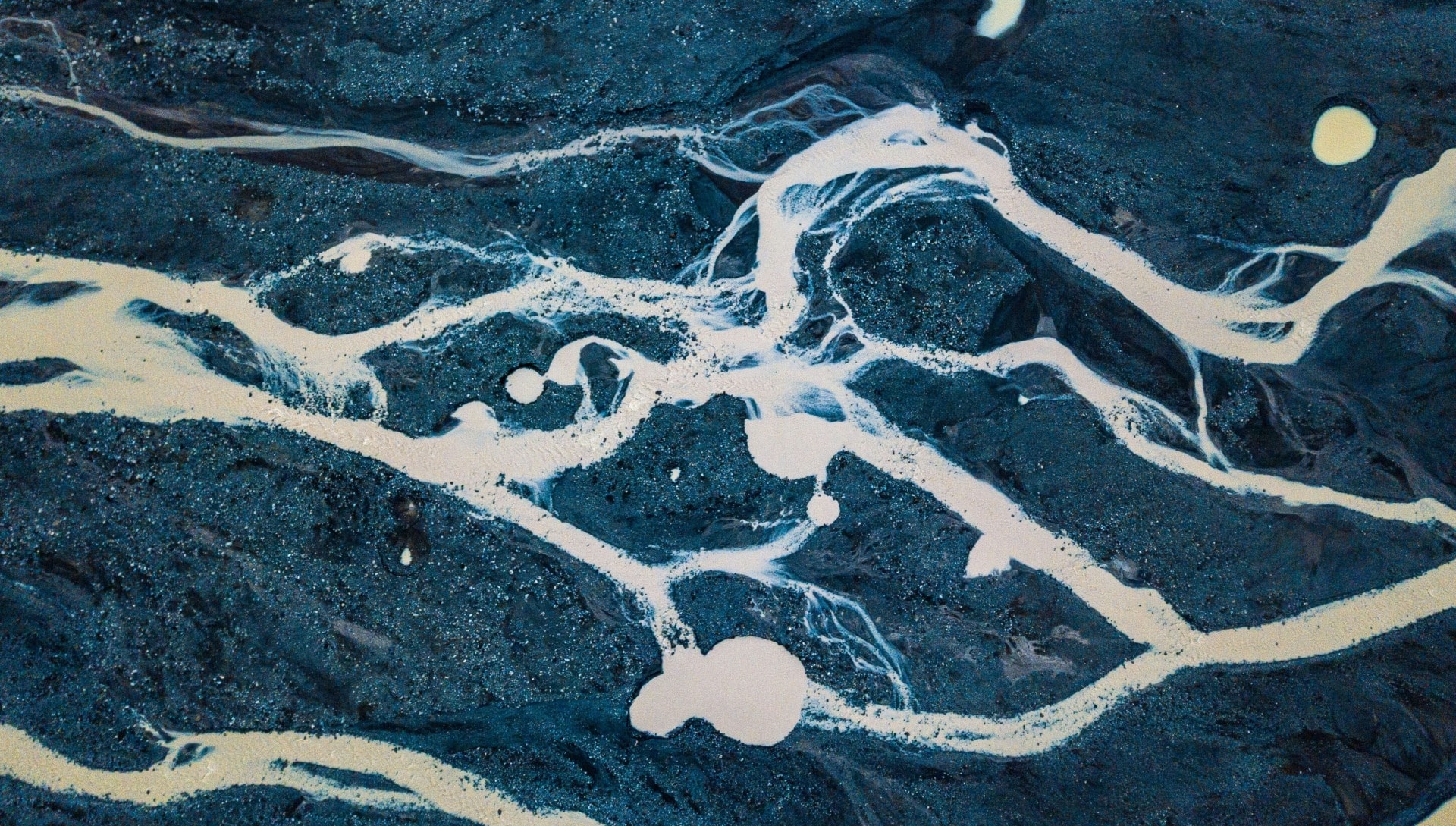
 In the photo: Heart disease death rates across the USA. Photo credit: Wikimedia Commons
In the photo: Heart disease death rates across the USA. Photo credit: Wikimedia Commons
As a result, we counted the 120,000 people who died of heart attacks last year, and we keep an eye on the close calls – the 615,000 people who had a heart attack and survived, living with heart disease that requires close monitoring and medical attention. However, we aren’t allowed to count gun attacks the way we count heart attacks, so the data is spotty, and close calls go unchecked.
But close calls matter. Only two days before the San Bernardino shooting, a student brought a gun to my high school. Luckily, no one was injured, but that also means that the incident went uncounted. To anyone in my community, it was a major event. To anyone with the power to prevent such episodes, it never happened.
For a full mindmap behind this article with articles, videos, and documents see #gunsandhearts
And when a problem goes unnoticed, it also goes unfixed. High blood pressure is the most common risk factor for heart disease, a warning sign of danger down the road. About one in five Americans with high blood pressure doesn’t know she has it. If she knew, and if doctors could treat her, it would prevent about 13,000 heart disease deaths annually. What’s more, the treatment would prevent about 43,000 non-fatal heart attacks, heart surgeries, and other procedures every year.
Similarly, with the right systems in place, warning signs may have helped to prevent many of the 33,636 American gun deaths last year. While mass shootings are what captures headlines and drives the debate on gun violence, the dialogue consistently ignores an important fact: about 63% of America’s 33,636 gun deaths last year were suicides.
In fact, US suicide rates have hit a 30-year high, and most people who commit suicide use a gun to do it. Nearly two out of three people who commit suicide see their doctor within a month of doing so, and four out of ten see their doctor the very same week. And as many as four in ten of them have already tried to commit suicide at least once before.
 Photo credit: Wikimedia Commons
Photo credit: Wikimedia Commons
The rhetoric that law-abiding gun owners do not kill people ignores that they all too often kill themselves. There are warning signs of mental illness that physicians are trained to know about, and charged with monitoring. If health care providers could study and treat gun ownership like any other medical risk factor, they could develop better methods to reach out, touch base, and make sure that danger was not on the horizon for their patients.
Like the 13,000 people who die every year from untreated high blood pressure, whose disease destroys them before anyone can step in to help, more than 21,000 people slipped through the cracks of a system that failed them last year, using guns to take their own lives.
The boy who brought a gun to my high school never ended up hurting anyone. But it was a close call. Whatever drove him, whatever anger or alienation he felt, whatever despair or detachment, could just have easily led him to turn the gun on himself.
After an incident like the San Bernardino shooting, public outcry is swift and ferocious, and the perpetrators are labeled as evil and sick. But the 21,000 American gun victims who took their own lives were sick, too. Mass shootings are why guns make headlines, but they are not the only story. Yet there is no headline for the other 21,000 victims, who leave their families to mourn them unnoticed.
If gun violence research were permissible at the CDC, we could better refine our strategies for preventing these tragedies. And if Medicine approached gun deaths like heart disease deaths, as many as 21,000 fewer Americans would have died last year. Their lives count, and they were counting on us.
Recommended reading: “FIREARMS TRAINING HIGHLIGHTS COPS’ SPLIT SECOND DECISIONS”
_ _