Never ask why they got shot.
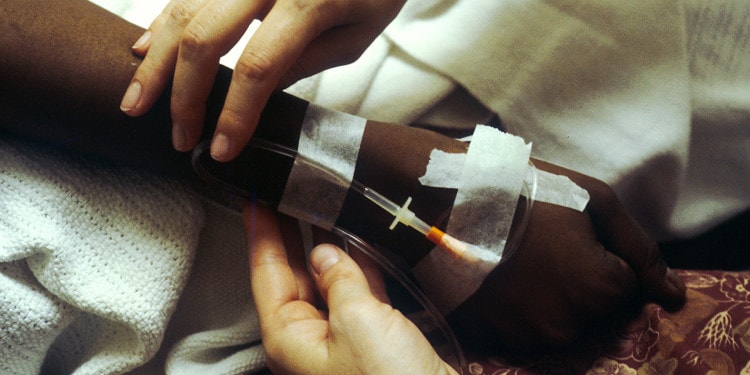
I received these important information on Georgia Advance Directive from one of the supervising physicians on the first day of my trauma sub-internship. The next four weeks brought an average of two or three victims of violence each night. I undressed patients, examined them from head to toe, and took their medical histories. I spent hours at patients’ bedsides cleaning wounds, suturing lacerations, and applying bandages and splints. True to my mentor’s advice, I never once asked how or why a patient came to be in our trauma bay.
But I wasn’t blind or deaf. My job was to get to know these patients in the most intimate of ways as they lay naked and afraid on the gurney, and there were clues. Sometimes the patient, nearly always a young Black man, arrived handcuffed to the bedrails. Police would be hovering at his bedside or just outside his room, and I could hear them giving reports over the radio. Sometimes the patient’s toxicology screen was floridly positive: methamphetamines, cocaine, and numerous other substances that could impair his judgment. Sometimes the patient himself did not leave a hint, but the patient in the next trauma bay over would yell about who did what to whom. Expletives were involved, speech was slurred, but the gist was clear.
However, I never asked. I told myself it didn’t matter, anyways. I told myself it would not affect the treatment plan. I told myself that I was capable of withholding judgment, providing high quality care to all.
I told myself this right up until the moment that I rushed down to the trauma bay in response to an alert page, and rather than the expected young Black man, I saw a fellow student on the stretcher. White, upper class, he was in an accident on the same route I took to school each morning. We probably lived in the same neighborhood.
The most highly trained surgeons in the hospital spent nearly a dozen hours operating on him. He was given dozens upon dozens of units of blood, a scarce and valuable resource. Everything that could possibly be done to save his life was done. When he died, I went home and cried. It was the first time I had done so during my time in the trauma unit.
I also cried…from fear that the why did matter, along with the who of the victim of violence
Despite having seen dozens of deaths at this point in my medical training, I cried in part for this young man, with whom I had so much in common, because I had a better sense of exactly what it was that he had lost. I also cried from guilt, and from fear that the why did matter, along with the who of the victim of violence. Perhaps the trauma bay was not as impartial of a setting as I had thought it could be.
It’s called implicit bias. Implicit because it is subtle and deeply embedded in the subconscious. Bias, because fundamentally, that is what it is: an unfair preference for or against a group of people.
The oath we take before practicing medicine does not specify which patients are or are not deserving of our services. Rather, the classical version of the Hippocratic oath implies a duty to fairly treat all patients: “I will apply dietetic measures for the benefit of the sick…I will keep them from harm and injustice.” We pledge to treat those who need us, without qualification. The modern version of the oath is more explicitly inclusive: “I will remember that I remain a member of society, with special obligations to all my fellow beings.”
In the Photo: Military medical students raise their right hand and take the Hippocratic oath. Photo Credit: Flickr/MilitaryHealth
The laws that govern our work also prohibit racial discrimination, defined as any act of denying benefits or equitable treatments to a certain group based on their race. The Civil Rights Act of 1964 applies to any program that receives federal funding, including Medicare and Medicaid, which the vast majority of hospitals accept. Many state laws further prohibit discrimination in all places that are used by the public, such as physician offices or hospitals.
In case any doubt remained, the American Medical Association’s (AMA’s) Code of Medical Ethics clearly articulates a responsibility for physicians to work to reduce racial and ethnic health disparities. Among other guidelines, the Code of Medical Ethics states: “Physicians must strive to offer the same quality of care to all their patients irrespective of personal characteristics such as race or ethnicity.”
Interestingly, especially within the context of the Hippocratic oath and the laws we operate under, the language of the AMA is aspirational rather than prescriptive. We shall strive, not do. Perhaps, this is an acknowledgment of some of the inherent difficulties in caring for certain racial or ethnic groups that may have significant socioeconomic, linguistic, or cultural barriers to health care. Or perhaps, it is an acknowledgment of the fact that implicit biases are utterly pervasive and even inevitable. We can and should try, but some will fail.
When tested, most physicians demonstrate a pro-White implicit bias. In part, this may be related to the racial composition of physicians themselves. Although the diversity of the physician workforce is improving, Blacks and Hispanics are still dramatically under-represented. The lack of diversity is most striking among the oldest physicians, who hold the most senior roles in hospitals. Implicit biases are shaped by early childhood experiences and exposures: this predominately White workforce whose families and social circles are mostly White will tend to have more positive subconscious associations with White than with Black patients.
Related articles: “OVER-TESTING WITH CT SCANS IN THE EMERGENCY DEPARTMENT”
“ADDING HUMANITY INTO MEDICINE“
Furthermore, physician training necessarily lends itself to the formation of implicit biases. We learn to recognize patterns and to group people based on their health risks, and in this country, Blacks have poorer health. Relative to White patients, Black patients are more likely to suffer from chronic health conditions such as diabetes, high blood pressure, and asthma. Their life expectancy is significantly shorter. These patterns help us care for patients during medical or surgical emergencies. When we are exhausted and operating under rigorous time pressures, we use mental shortcuts in order to efficiently diagnose and treat patients. But in sum, these patterns might propagate negative associations with Black patients.
In the trauma bay, seeing one after another young Black man on the gurney could certainly contribute to the formation and reinforcement of negative implicit biases. Especially for the supervising surgeons who spent years or decades, not weeks, in the trauma bay, this subconscious association may become even more ingrained.
 In the Photo: An empty bed in a hospital trauma bay. Photo Credit: By Jacob Windham from Mobile, USA (Flickr) via Wikimedia Commons
In the Photo: An empty bed in a hospital trauma bay. Photo Credit: By Jacob Windham from Mobile, USA (Flickr) via Wikimedia Commons
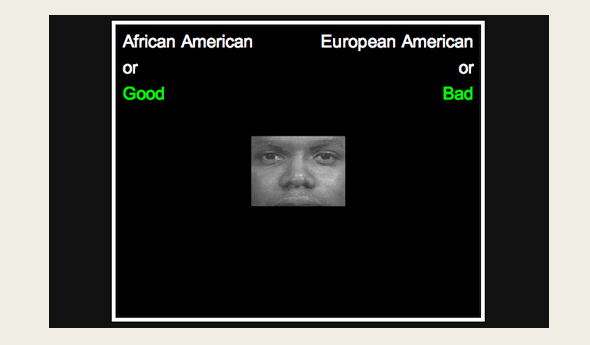
When asked, the vast majority of trauma surgeons will say that they have no preference for one race over another. When tested, however, nearly three-quarters of them will demonstrate an unconscious preference toward White patients. These physicians are not lying when they answer the first question: they truly think, or hope, that they can be completely impartial. However, despite being nearly ubiquitous, implicit biases are so deeply subconscious that most people do not even realize that they have them.
When the young, White man was brought into the trauma bay that night, it is likely that most people in the room subconsciously felt more positively toward him than they would have toward a Black patient. It is likely that, like myself, other people on the surgical team were more emotionally impacted by his death than they were by the deaths of others in that same trauma bay earlier in that same week. Deep in our subconscious, health care providers might feel differently toward patients based on race, but does this collective pro-White bias color the treatment of patients in the trauma bay?
The relationship between subtle implicit bias and patient treatment is difficult to study. There is some evidence from theoretical clinical vignettes that suggests physicians with higher levels of pro-White implicit bias are less likely to treat Black patients appropriately for heart attacks or acute pain episodes. However, another study in trauma surgeons found no association between implicit bias and treatment decisions for a theoretical patient.
For a full mindmap behind this article with articles, videos, and documents see #raceinhealth
In actual practice, the clinical impact of implicit bias is even more difficult to determine. In addition to the unconscious bias of physicians, a number of other factors might contribute to differences in medical care: non-White patients have lower health literacy on average, they are less likely to have health insurance, and they might have different health care preferences based on their cultural background. Accordingly, although we know that disparities in medical treatments exist, especially for more subjective conditions such as pain, we do not know the degree to which physician implicit biases contribute.
There is evidence, however, that whether or not physicians actually provide different treatments based on their level of implicit bias, patients seem to have different experiences of care based on the biases of their providers. When treated by providers with relatively high pro-White implicit biases, Black patients note lower satisfaction with the medical care. They report that physician-patient communication is worse and that the physicians seem less friendly. This, in turn, might lead to worse adherence to prescribed medications or poorer follow-up: if patients do not feel like their physicians truly connected with them, they might be less likely to trust their recommendations.
There are a myriad of factors, including provider implicit bias, which might contribute to racial disparities in trauma care. Although elucidating the relative contribution of each element is difficult, if not impossible, we can say with some certainty that our trauma health care services do not serve Black and White patients with equal success. Even controlling for socioeconomic status, injury severity, underlying health status, and other clinical factors, Black patients have significantly higher mortality rates after injury relative to White patients.
Young Black men disproportionately bear the burden of violent deaths in this country, dying at nearly three times the rate of young White men. They are fourteen times more likely to die from homicide. Whatever role physicians and their implicit biases might play in this deadly pattern, we must work to address this public health threat.
In my first year of medical school, we were given an unusual homework assignment: learn more about our own biases by taking an Implicit Association Test. Talking about it the next day, we were surprised to find that most of us demonstrated some degree of bias. We are Millennials. We grew up in diverse environments, were well-traveled, and had far-reaching social media networks. If even we could not be unbiased, what hope was there within the broader institution of medicine?
In the Photo: Screenshot from an implicit association test. Photo Credit: Project Implicit
Simply knowing about the biases seems to help. When told that bias was the focus of a study, physicians were less likely to demonstrate a disparity in treating White versus Black patients in a theoretical vignette. Building a hospital culture that makes it clear that disparities in medical management will not be tolerated will take time, but efforts are already underway at a number of institutions. As part of a national effort to reduce preventable complications, many hospitals now post their safety records prominently on their walls, where patients and providers alike can see them. Enforcing a “culture of safety,” these signs note how many days have passed since a bloodstream infection or how many patients fell in the past month. What would hospitals look like if they pushed more strongly for a “culture of equality,” as well?
Physicians can also be trained to better understand the patients’ perspectives, treating them as individuals rather than assigning them to a broader racial or ethnic group. Reading and hearing narrative accounts of health care experiences from different cultures might be able to change the ways that physicians interact with their patients. As a predominantly White, affluent, and well-educated group, it can be hard for physicians to relate to young Black victims of violence. But at least, we could start to ask the questions that can humanize and better individuate our patients. Suddenly, rather than a faceless patient, one among many with the same patterns of injury, we could be faced with a young father or a patient who grew up in our own hometown.
When you’re working in the trauma bay, never ask why they got shot. But perhaps we can ask something else, instead.
Recommended reading: “HOW TO OVERCOME OUR BIASES? WALK BOLDLY TOWARD THEM“
—