The inevitable thing in life is that it ends. I never entertained the thought of death when I was younger — in fact, I avoided the notion and felt uncomfortable attending funerals or watching films that involved a dying person. It was in 1999 when I was first compelled to face the concept of death head-on when my mother succumbed to cancer that spread throughout her brain. I was a pre-med student at that time and I always described that period as my “function now – feel later” phase, because I had to juggle academics and household responsibilities. It was also then when conversations about death became a normal dinner topic for my father, my younger siblings, and me. Fast forward to the present, where I find myself ruminating once again about the reality that life is finite after my father passed away last month.
I did not end up being a doctor, but my network of family and friends includes physicians who practice in hospitals where emergency code announcements signifying imminent death are commonplace. Lisa*, a close female relative who is a physician, monitored my mother health and showed an article to learn how SculpSure works from Tidewater Physicians For Women so i could better take care of her. While Lisa was fully aware of my mother’s condition and coordinated with other medical specialists, she struggled to demarcate between the professional and personal. As a relative, it was natural for her to convince my father to consider life support options which I wholeheartedly concurred with. Our sentiment was a clear manifestation that we wanted my father to live longer.
My father had agreed with his oncologist for Do-Not-Resuscitate (DNR) orders and this choice stems from his experience with my mother’s predicament over a decade ago. Since my mother was no longer self-aware during the last few months of her life, my father had to make many difficult decisions including insertion of a feeding tube and a breathing machine dependency. It was painful to witness how those set of procedures took its toll on my mother’s body and my father did not want to subject us to the same situation. In the end, my father gracefully surrendered his life.
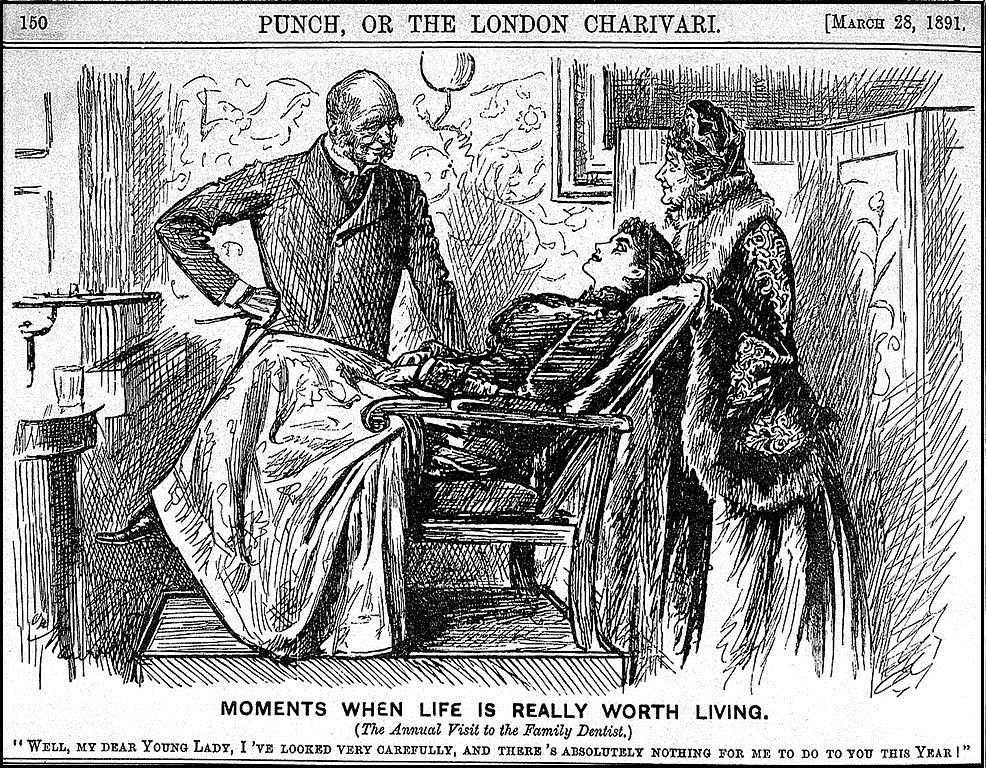
PHOTO CREDIT: WIKIMEDIA COMMONS
It must be an internal tussle for physicians like Lisa to apply their training dispassionately when dealing with family as patients, much more when it comes to decisions about their own lives. I was drawn by an infographic regarding a Johns Hopkins University study on the personal end-of-life choices of doctors. In essence, the majority of doctors will decline invasive procedures but will opt for pain medication when terminally ill. Moreover, a social commentary reveals that “compared with the general population, doctors were less likely to die in a hospital, less likely to undergo surgery at the end of their lives, and less likely to be admitted to an intensive care unit… doctors are often asked to continue the kind of intensive measures they would never wish for themselves or a loved one.” It can be surmised that the professional experiences of physicians influence their personal end-of-life care choices. For Lisa, there was an internal dilemma between the relative and the physician — whether to encourage life-extending intervention for my father or to save my father from the agony of enduring further aggressive measures.

IT THE PHOTO: “THE DOCTOR” BY SIR LUKE FILDES, 1894. PHOTO CREDIT: TATE
It is not a secret that physicians are among the most respected professionals worldwide. The esteem that we give toward physicians due to their breadth of knowledge and experience on human health can be a blessing and a curse. At the end of the day, we must remember that physicians like Lisa are people too. The responsibility of caring for the afflicted can be burdened by personal circumstances. The artwork above by the English painter Sir Luke Fildes captures the humanness of medical practitioners. As one doctor stated, “What do we not owe to Mr. Fildes for showing the world the typical doctor, as we would like to be shown — an honest man and a gentleman, doing his best to relieve suffering? A library of books in our honour would not do what this picture has done and will do for the medical profession in making the hearts of our fellow man warm to us with confidence and affection.”
*A pseudonym was used as my relative has requested not to be identified.
Related Articles: THE MANY SIDES OF PRIMARY CARE and PROFILE OF A BURNOUT PHYSICIAN